Trong cuộc sống, khi gặp khó khăn và cảm thấy cô đơn, hãy để những hình ảnh này làm bạn đồng cảm và tìm thấy sự đồng điệu với tâm trạng của mình.
Những bức ảnh buồn, cô đơn này sẽ làm bạn cảm thấy nhẹ nhàng hơn, hãy tải về và chia sẻ để người thân hiểu rõ hơn về tâm trạng của bạn.

Hơn 100 hình ảnh buồn, cô đơn đẹp mắt giúp bạn có nhiều sự lựa chọn để thể hiện đúng tâm trạng của mình.

Khám Phá Nỗi Lẻ Lẻo, Hình Ảnh Buồn 1

Hình Ảnh Cô Đơn, Bước Nhẹ 2

Góc Khuất Của Nỗi Buồn, Hình Ảnh Cô Đơn 3
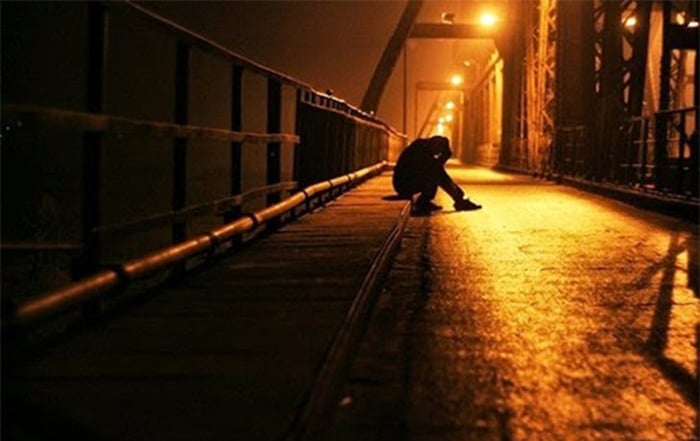
Chạm Nhẹ Nỗi Đau, Hình Ảnh Buồn 4

Dấu Chân Cô Đơn, Hình Ảnh Buồn 5

Khung Cảnh Nỗi Lẻ Lẻo, Cô Đơn 6

Góc Khuất Của Nỗi Buồn, Hình Ảnh Cô Đơn 7

Chạm Nhẹ Nỗi Đau, Hình Ảnh Buồn 8

Điệu Nhảy Cô Đơn, Hình Ảnh Buồn 10

Lời Hứa Lạc Lõng, Hình Ảnh Buồn 11

Bước Chân Đơn Độc, Cảm Xúc Cô Đơn 12

Khung Cảnh Nỗi Buồn, Hình Ảnh Buồn 13

Đêm Lạnh Buốt, Hình Ảnh Cô Đơn 14

Hình Ảnh Thất Tình, Cảm Xúc Cô Đơn 15

Bước Chân Lạc Lõng, Hình Ảnh Buồn 16

Nỗi Lẻ Loi, Góc Khuất Cô Đơn 17

Đêm Sâu Thẫn Thờ, Hình Ảnh Buồn 18

Nỗi Lẻ Loi, Cảm Xúc Cô Đơn 19

Bóng Đêm Thấp Thoáng, Hình Ảnh Cô Đơn 20

Khóc Lặng Lẽ, Góc Cô Đơn 21

Góc Hình Ảnh Buồn, Nỗi Lẻ Loi 22
Bức Hình Thất Tình, Cô Đơn 23

Lạc Trôi Nơi Ảo Ảnh, Hình Ảnh Cô Đơn 24

Hình Ảnh Buồn, Cô Đơn 25 - Bóng Đêm Thầm Lặng

Nỗi Lạc Lõng, Góc Tối Của Cô Đơn 26

Ánh Sáng Yếu Đuối, Cảm Xúc Cô Đơn 27

Đêm Buông Lơi, Hình Ảnh Cô Đơn 28

Lạc Trôi Trong Nỗi Buồn, Cô Đơn 29

Nỗi Buồn Sâu Thẳm, Hình Ảnh Cô Đơn 30

Khói Lửa Nỗi Buồn, Hình Ảnh Cô Đơn 31

Hình Ảnh Buồn, Cảm Xúc Cô Đơn 32

Góc Tối Cô Đơn, Hình Ảnh Buồn 33

Góc Tối Cô Đơn, Hình Ảnh Buồn 34

Nỗi Buồn Lặng Lẽ, Hình Ảnh Cô Đơn 35

Dấu Vết Nước Mắt, Hình Ảnh Cô Đơn 36

Góc Tối Cô Đơn, Hình Ảnh Buồn 37

Hình Ảnh Đau Đớn, Góc Lạc Lõng 38

Cảm Xúc Khó Diễn Đạt, Hình Ảnh Cô Đơn 39

Dấu Ấn Cô Đơn, Hình Ảnh Buồn 40

Bóng Tối Đầy Nặng, Cô Đơn 41

Hình Ảnh Buồn, Cảm Xúc Đau Đớn 42

Bức Hình Thất Tình, Cô Đơn 43

Lạc Trôi Nơi Ảo Ảnh, Hình Ảnh Cô Đơn 44

Hình Ảnh Buồn, Cô Đơn 45 - Đêm Trầm Lặng

Bóng Tối Kín Đáo, Hình Ảnh Cô Đơn 46

Nỗi Buồn Nén Lòng, Hình Ảnh Cô Đơn 47

Không Gian Hư Ảo, Hình Ảnh Cô Đơn 48
Nỗi Lòng Hẹn Hò, Góc Cô Đơn 49

Lạnh Lẽo Đêm Đen, Hình Ảnh Cô Đơn 50

Bước Chân Lạc Lõng, Hình Ảnh Cô Đơn 51

Đong Đầy Nỗi Nhớ, Góc Cô Đơn 52

Ánh Đèn Mờ Nhạt, Hình Ảnh Cô Đơn 53

Khói Lửa Tình Phai, Góc Cô Đơn 54
Hương Thơm Mưa Rơi, Hình Ảnh Cô Đơn 55

Vết Thương Không Nguôi, Hình Ảnh Cô Đơn 56

Đêm Dài Hối Hả, Góc Cô Đơn 57

Đêm Buồn Mưa Rơi, Góc Cô Đơn 58

Hình Ảnh Lạc Lõng, Cô Đơn 59

Bước Chân Lạc Lõng, Hình Ảnh Cô Đơn 60

Khói Sương Mỏng Manh, Góc Cô Đơn 61

Ký Ức Buồn, Nỗi Cô Đơn 62

Chạm Nhẹ Hình Bóng, Cảm Giác Cô Đơn 63

Lạc Lõng Trong Đêm, Hình Ảnh Buồn 64

Góc Khuất Cô Đơn, Đêm Dài 65

Nỗi Buồn Vô Hình, Đêm Đen 66

Cảm Xúc Lạc Lõng, Góc Tối 67

Hình Ảnh Cô Đơn, Điệu Nhảy Mưa 68

Đêm Buông Lơi, Bóng Tối Khuất 69
Khung Cảnh Hụt Hẫng, Đêm Tịch Tĩnh 70

Lặng Lẽ Hối Tiếc, Đóa Hồng Khô 71

Nén Nỗi Buồn, Đường Mòn Lạc Lõng 72

Cô Đơn Nơi Xa Lạ, Đèn Đường Ẩn 73

Góc Phố Lạnh Lẽo, Nắng Ẩn 74

Bước Chân Cô Đơn, Hạt Mưa Lạc Loài 75

Cảnh Hoàng Hôn Cô Đơn, Lá Phai Màu 76

Khói Thuốc Lạc Lõng, Cây Cầu Nối 77

Lạc Lõng Trong Dòng Đời, Nỗi Buồn 78

Đêm Sâu Thẳm, Hình Ảnh Cô Đơn 79

Góc Phố Hoang Vu, Những Ký Ức 80

Ngọn Đèn Dầu Cô Đơn, Cõi Lòng 81

Buổi Sáng Mơ Mộng, Cảm Xúc Cô Đơn 82

Nỗi Lòng Buồn, Góc Phố Cô Đơn 83
Khói Sương Mỏng, Hình Ảnh Buồn 84

Dòng Sông Cô Đơn, Bóng Đêm Ẩn Mình 85

Khung Cảnh Cô Đơn, Nỗi Lòng Ẩn Trong 86

Bức Tranh Buồn, Hình Ảnh Lạc Lõng 87
Cảm Xúc Cô Đơn, Đêm Dài Thẻo 88

Nỗi Nhớ Quê Hương, Ánh Đèn Sáng Lấp Lánh 89

Khung Cảnh Cô Đơn, Bóng Tối Đậm Đặc 90

Hình Ảnh Buồn, Cô Đơn 91 - Cõi Lạc Lõng

Cảm Xúc Đơn Độc, Nỗi Buồn Thấu Tận Tâm Hồn 92

Hình Ảnh Lẻ Loi, Cô Đơn Nơi Đâu 93

Lạc Lõng Giữa Đêm Buồn, Hình Ảnh Cô Đơn 94

Khám Phá Nỗi Buồn, Hình Ảnh Cô Đơn 95

Bước Chân Cô Đơn Trên Con Đường Ảo 96

Nơi Đâu Còn Đây, Hình Ảnh Buồn, Cô Đơn 97

Góc Tối Huyền Bí, Hình Ảnh Cô Đơn 98

Dấu Chân Mưa, Hình Ảnh Buồn, Cô Đơn 99

Hành Trình Cô Đơn Trong Đêm U Tối 100

Lạc Lõng Trong Hư Vô, Hình Ảnh Cô Đơn 101

Chập Tắt Ánh Sáng, Hình Ảnh Buồn, Cô Đơn 102

Góc Phố Hoang Vắng, Hình Ảnh Cô Đơn 103

Nhìn Lên Bầu Trời Đêm, Hình Ảnh Buồn, Cô Đơn 104

Lạc Lõng Giữa Đại Dương Emptiness, Hình Ảnh Cô Đơn 105

Bước Chân Đơn Độc Trên Con Đường Mưa, Hình Ảnh Buồn 106

Nỗi Lặng Cô Đơn, Ánh Đèn Dịu Dàng, Hình Ảnh Buồn 107

Góc Phố Hoang Vắng, Nỗi Buồn Thấp Thỏm 108
Chạm Nhẹ Hương Sầu, Hình Ảnh Buồn, Cô Đơn 109

Khóc Lặng Trong Sự Cô Đơn
Dưới đây là bộ sưu tập hình ảnh cô đơn và buồn, hy vọng bạn sẽ tìm thấy niềm vui trong cuộc sống và bước qua cảm giác cô đơn. Chúc bạn luôn hạnh phúc!