Dr.Fawaz al sarayreh lecture
https://youtu.be/Do9LfxMrqB8
Basic Knowledge
Structure: The uveal tract (also known as the vascular pigmented layer, vascular tunic, and uvea) takes its name from the Latin uva (grape) because the dark pigmentation and shape of the structure are reminiscent of a grape. The uveal tract consists of the following structures:
- Iris,
- Ciliary body,
- Choroid.
Position: The uveal tract lies between the sclera and retina.
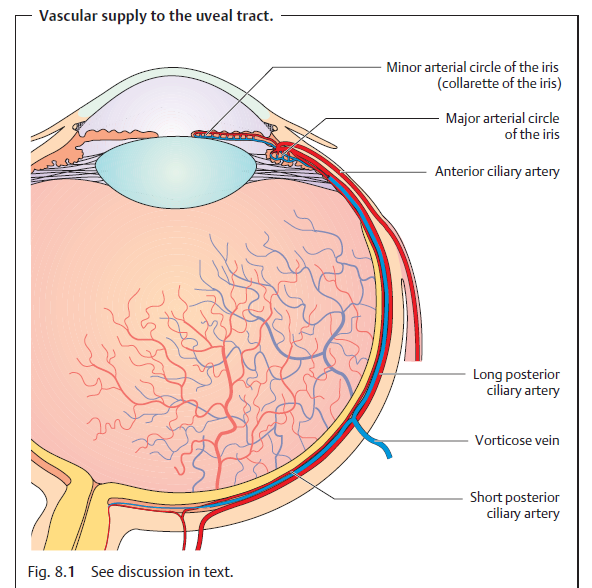
Neurovascular supply: Arterial supply to the uveal tract is provided by the ophthalmic artery. The short posterior ciliary arteries enter the eyeball with the optic nerve
and supply the choroid. The long posterior ciliary arteries course along the interior surface of the sclera to the ciliary body and the iris. They form the major arterial circle at the root of the iris and the minor arterial circle in the collarette of the iris. The anterior ciliary arteries originate from the vessels of the rectus muscles and communicate with the posterior ciliary vessels.
Venous blood drains through four to eight vorticose or vortex veins that penetrate the sclera posterior to the equator and join the superior and inferior ophthalmic veins. Sensory supply is provided by the long and short ciliary nerves.
Iris
Structure and function: The iris consists of two layers:
- The anterior mesodermal stromal layer.
- The posterior ectodermal pigmented epithelial layer. The posterior layer is opaque and protects the eye against excessive incident light. The anterior surface of the lens and the pigmented layer are so close together near the pupil that they can easily form adhesions in inflammation.
- The collarette of the iris covering the minor arterial circle of the iris divides the stroma into pupillary and ciliary portions. The pupillary portion contains the sphincter muscle, which is supplied by parasympathetic nerve fibers, and the dilator pupillae muscle, supplied by sympathetic nerve fibers. These muscles regulate the contraction and dilation of the pupil so that the iris may be regarded as the aperture of the optical system of the eye.
- Pupil dilation is sometimes sluggish in preterm infants and the newborn because the dilator pupillae muscle develops relatively late.
- Surface: The normal iris has a richly textured surface structure with crypts (tissue gaps) and interlinked trabeculae. A faded surface structure can be a sign of inflammation (see iridocyclitis).
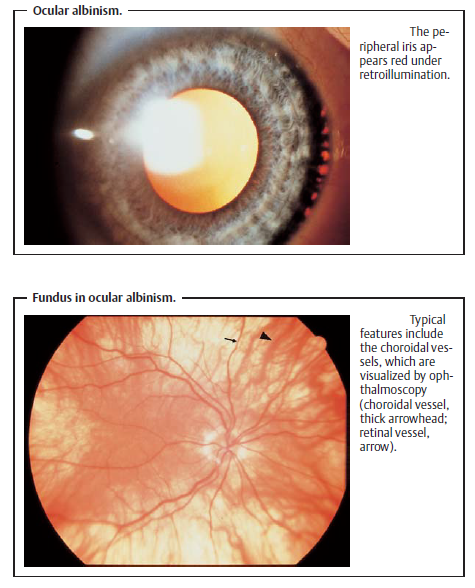
- Color: The color of the iris varies in the individual according to the melanin content of the melanocytes (pigment cells) in the stroma and epithelial layer. Eyes with a high melanin content are dark brown, whereas eyes with less melanin are grayish-blue. Caucasians at birth always have a grayish-blue iris as the pigmented layer only develops gradually during the first year of life. Even in albinos (see impaired melanin synthesis), the eyes have a grayish blue iris because of the melanin deficiency. Under slit lamp retro-illumination they appear reddish due to the fundus reflex.
Ciliary Body
- Position and structure: The ciliary body extends from the root of the iris to the ora serrata, where it joins the choroid. It consists of anterior pars plicata and the posterior pars plana, which lies 3.5mm posterior to the limbus. Numerous ciliary processes extend into the posterior chamber of the eye. The suspensory ligament, the zonule, extends from the pars plana and the intervals between the ciliary processes to the lens capsule.
- Function: The ciliary muscle is responsible for accommodation. The double layered epithelium covering the ciliary body produces the aqueous humor.
Choroid
Position and structure: The choroid is the middle tunic of the eyeball. It is bounded on the interior by Bruch’s membrane. The choroid is highly vascularized, containing a vessel layer with large blood vessels and a capillary layer. The blood flow through the choroid is the highest in the entire body.
Function: The choroid regulates temperature and supplies nourishment to the outer layers of the retina.
Developmental Anomalies
Aniridia
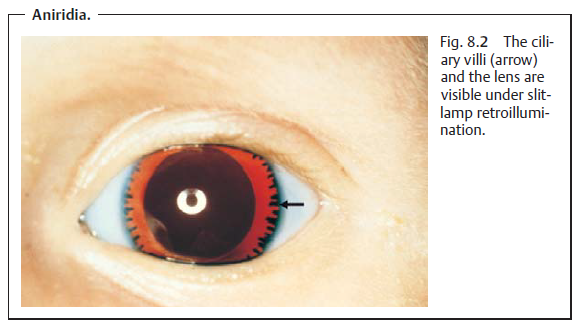
Aniridia is the absence of the iris. This generally bilateral condition is transmitted as an autosomal dominant trait or occurs sporadically. Aniridia may also be traumatic and can result from penetrating injuries. However, peripheral remnants of the iris are usually still present so that ciliary villi and zonule fibers will be visualized under slit-lamp examination. In sporadic aniridia, a Wilms’ tumor of the kidney should be excluded. Vision is severely compromised as a result of the foveal hypoplasia. The disorder is frequently associated with nystagmus, amblyopia, buphthalmos, and cataract. Visual acuity will generally be reduced in the presence of nystagmus.
Coloboma
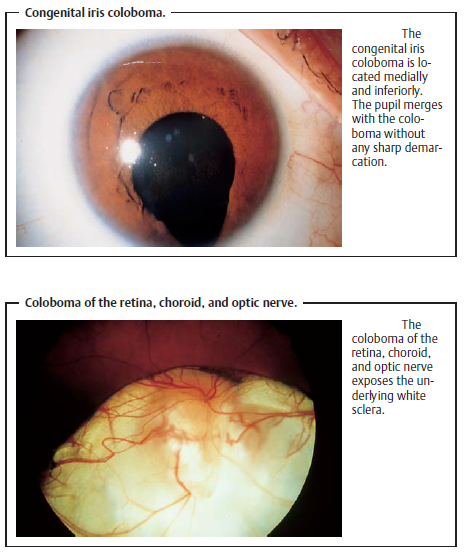
Another congenital anomaly results from incomplete fusion of the embryonic optic cup, which normally occurs in about the sixth week of pregnancy. These anomalies are known as colobomas. They are directed medially and inferiorly and can involve the iris, ciliary body, zonule fibers, choroid, and optic nerve. Bridge colobomas exhibit remnants of the iris or choroid. Involvement of the choroid and optic nerve frequently leads to reduced visual acuity. Surgical iris colobomas in cataract and glaucoma surgery are usually opened superiorly. In this manner, they are covered by the upper eyelid so the patient will not usually experience blinding glare. Traumatic iris colobomas are caused by avulsion of the iris
Pigmentation Anomalies
Heterochromia
Impaired development of the pigmentation of the iris can lead to a congenital difference in coloration between the left and right iris (heterochromia). One iris containing varying pigmentation is referred to as iris bicolor. Isolated heterochromia is not necessarily clinically significant (simple heterochromia), yet it can be a sign of abnormal changes. The following types are differentiated:
- Fuchs’ heterochromic cyclitis (etiology unclear): This refers to recurrent iridocyclitis (simultaneous inflammation of several portions of the uveal tract) in adults, with precipitates on the posterior surface of the cornea without formation of posterior synechiae (adhesions between the iris and lens). The eye is free of external irritation. This disorder is often associated with complicated cataract and increased intraocular pressure (glaucoma).
- Sympathetic heterochromia: In unilateral impairment of the sympathetic nerve supply, the affected iris is significantly lighter. Heterochromia with unilaterally lighter pigmentation of the iris also occurs in iridocyclitis, acute glaucoma, and anterior chamber hemorrhage (hyphema).
- Melanosis of the iris: This refers to dark pigmentation of one iris. Aside from the difference in coloration between the two irises, neither sympathetic heterochromia nor melanosis leads to further symptoms. The only form of heterochromia that leads to abnormal changes is Fuchs’ heterochromic cyclitis. The possible complications involved require specific treatment.
Albinism
Albinism (from the Latin albus = white) is a congenital metabolic disease that leads to hypopigmentation of the eye. The following types are differentiated:
- ocular albinism (involving only the eyes) and
- oculocutaneous albinism (involving the eyes, skin, and hair).
In albinism the iris is light blue because of the melanin deficiency resulting from impaired melanin synthesis. Under slit-lamp retroillumination, the iris appears reddish due to fundus reflex (Fig. 8.6). Ophthalmoscopy will detect choroidal vessels. Associated foveal aplasia results in significant reduction in visual acuity and nystagmus. Most patients are also photophobic because of the missing filter function of the pigmented layer of the iris.
https://web.facebook.com/khalil.alsalem/videos/10159206271600608/?t=2
Inflammation
Inflammations of the uveal tract are classified according to the various portions of the globe:
- Anterior uveitis (iritis).
- Intermediate uveitis (cyclitis).
- Posterior uveitis (choroiditis). However, some inflammations involve the middle portions of the uveal tract such as iridocyclitis (inflammation of the iris and ciliary body) or panuveitis (inflammation involving all segments).
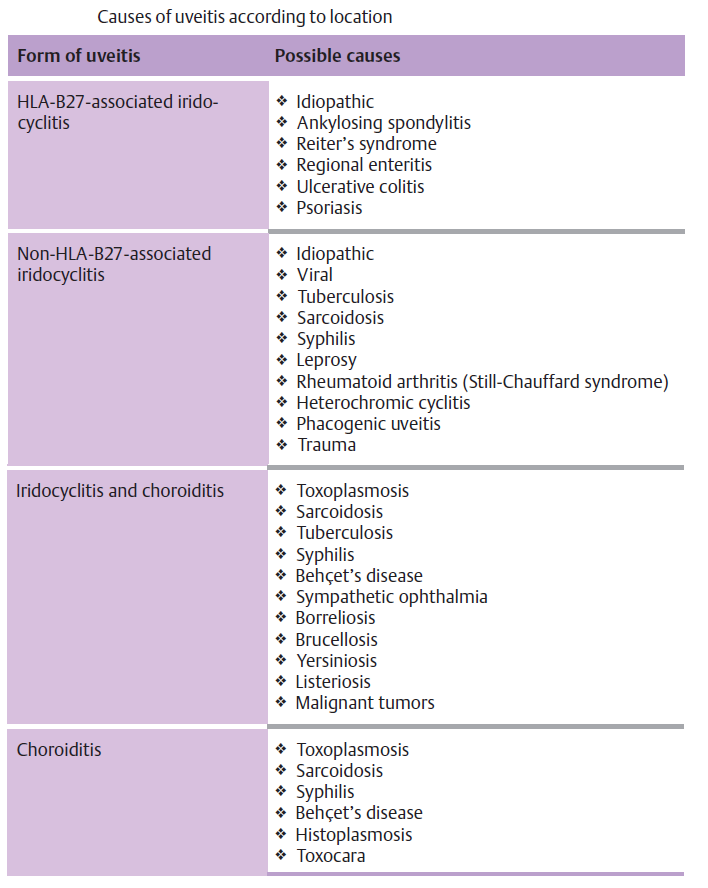
Acute Iritis and Iridocyclitis
Epidemiology: Iritis is the most frequent form of uveitis. It usually occurs in combination with cyclitis. About three-quarters of all iridocyclitis cases have an acute clinical course. Etiology: Iridocyclitis is frequently attributable to immunologic causes such as allergic or hyperergic reaction to bacterial toxins. In some rheumatic disorders it is known to be frequently associated with the expression of specific human leukocyte antigens (HLA) such as HLA-B27. Iridocyclitis can also be a symptom of systemic disease such as ankylosing spondylitis, Reiter’s syndrome, sarcoidosis, etc. (Table 8.1). Infections are less frequent and occur secondary to penetrating trauma or sepsis (bacteria, viruses, mycosis, or parasites). Phacogenic inflammation, possibly with glaucoma, can result when the lens becomes involved.
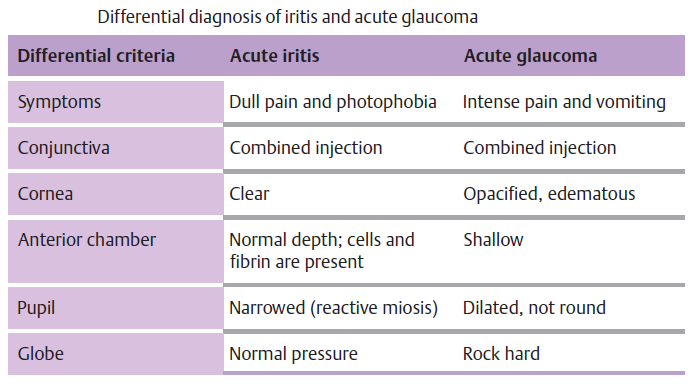
Symptoms: Patients report dull pain in the eye or forehead accompanied by impaired vision, photophobia, and excessive tearing (epiphora). In contrast to choroiditis, acute iritis or iridocyclitis is painful because of the involvement of the ciliary nerves.
Diagnostic considerations:
Typical signs include:
- Ciliary injection: The episcleral and perilimbal vessels may appear blue and red.
- Combined injection: The conjunctiva is also affected.
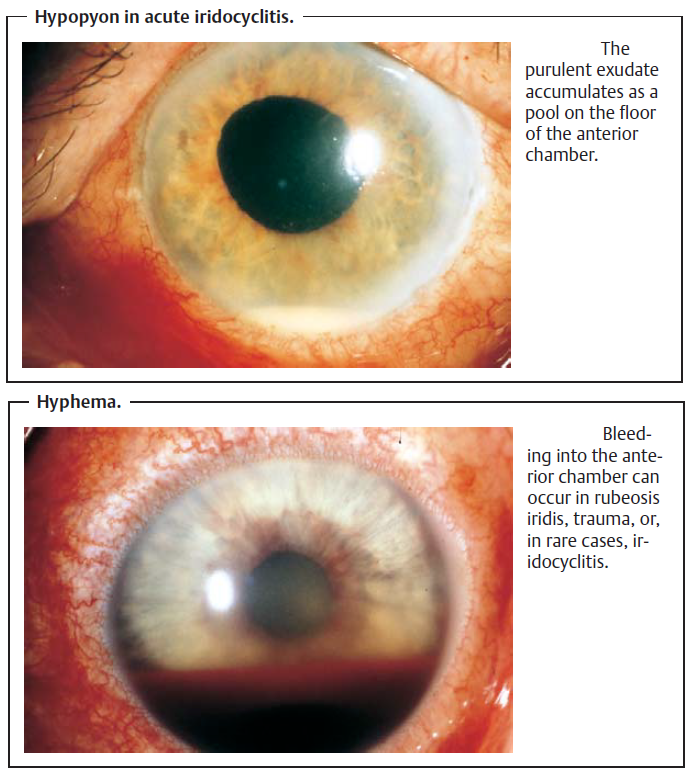
The iris is hyperemic (the iris vessels will be visible in a light-colored iris). The structure appears diffuse and reactive miosis is present. Vision is impaired because of cellular infiltration of the anterior chamber and protein or fibrin accumulation. Exudate accumulation on the floor of the anterior chamber is referred to as hypopyon. Viral infections may be accompanied by bleeding into the anterior chamber . Corneal edema can also develop in rare cases.
Complications:
- Secondary open angle glaucoma with an increase in intraocular pressure.
- Adhesions between the iris and posterior surface of the cornea (anterior synechiae).
- Adhesions between the iris and lens (posterior synechiae). Treatment: Topical and, in appropriate cases, systemic antibiotic or antiviral therapy is indicated for iridocyclitis due to a pathogen (with a corneal ulcer, penetrating trauma, or sepsis).
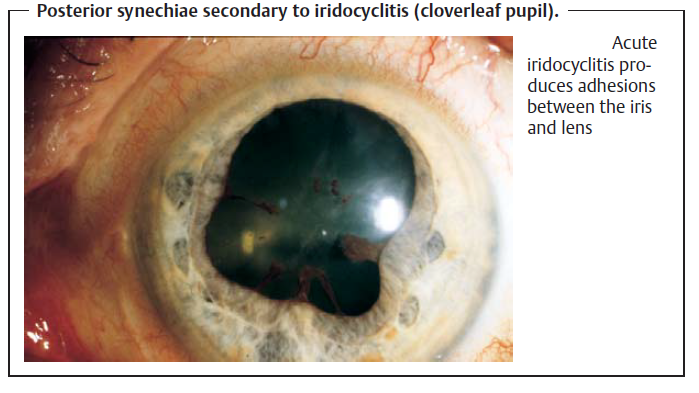
A conjunctival smear, or a blood culture in septic cases, is obtained to identify the pathogen. Antibiotic therapy should begin immediately as microbiological identification of the pathogen is not always successful. Therapeutic mydriasis in combination with steroid therapy is indicated to minimize the risk of synechiae. Where no pathogen can be identified, high-dose topical steroid therapy (prednisolone eyedrops every hour in combination with subconjunctival injections of soluble dexamethasone) is administered. Tominimize the risk of posterior synechiae, the pupil must be maximally dilated (atropine, scopolamine, cyclopentolate, and possibly epinephrine and epinephrine eyedrops). The mydriatic effect of dilating eyedrops may be reduced in iritis. This may necessitate the use of longer-acting medications such as atropine, which may have to be applied several times daily.
Occasionally it is possible to break off existing synechiae in this manner, and patches of iris tissue will remain on the anterior surface of the lens. Secondary open angle glaucoma is treated by administering beta blockers in eye drop form and, in applicable cases, carbonic anhydrase inhibitors (acetazolamide).
Prognosis: Symptoms usually improve within a few days when proper therapy is initiated. The disorder can progress to a chronic stage.
Chronic Iritis and Iridocyclitis
Epidemiology: About one quarter of all iridocyclitis cases have a chronic clinical course.
Etiology:
Symptoms: See acute iridocyclitis. Chronic iridocyclitis may exhibit minimal symptoms.
Diagnostic considerations: See acute iridocyclitis.
Differential diagnosis: The disorder should be distinguished from acute glaucoma, conjunctivitis, and keratitis.
Complications: Total obliteration of the pupil by posterior synechiae is referred to a pupillary block. Because the aqueous humor can no longer circulate, secondary angle closure glaucoma with iris bombé occurs. Occlusion of the pupil also results in fibrous scarring in the pupil. This can lead to the development of posterior subcapsular opacities in the lens (secondary cataract). Recurrent iridocyclitis can also lead to calcific band keratopathy.
Treatment: In pupillary block with a secondary angle closure glaucoma, a Nd:YAG laser iridotomy may be performed to create a shunt to allow the aqueous humor from the posterior chamber to circulate into the anterior chamber. In the presence of a secondary cataract, a cataract extraction may be performed when the inflammation has abated.
Prognosis: Because of the chronic recurrent course of the disorder, it frequently involves complications such as synechiae or cataract that may progress to blindness from shrinkage of the eyeball.
Choroiditis:
Epidemiology: There are few epidemiologic studies of choroiditis. The annual incidence is assumed to be four cases per 100 000 people.
Symptoms: Patients are free of pain, although they report blurred vision and floaters.
Choroiditis is painless as the choroid is devoid of sensory nerve fibers.
Diagnostic considerations: Ophthalmoscopy reveals isolated or multiple choroiditis foci. In acute disease they appear as ill-defined white dots . Once scarring has occurred the foci are sharply demarcated with a yellowish-brown color. Occasionally the major choroidal vessels will be visible through the atrophic scars.
No cells will be found in the vitreous body in a primary choroidal process. However, inflammation proceeding from the retina (retinochoroiditis) will exhibit cellular infiltration of the vitreous body.
Differential diagnosis: This disorder should be distinguished from retinal inflammations, which are accompanied by cellular infiltration of the vitreous body and are most frequently caused by viruses or Toxoplasma gondii.
Treatment: Choroiditis is treated either with antibiotics or steroids, depending on its etiology.
Prognosis: The inflammatory fociwill heal within two to sixweeks and form chorioretinal scars. The scars will result in localized scotomas that will reduce visual acuity if the macula is affected.
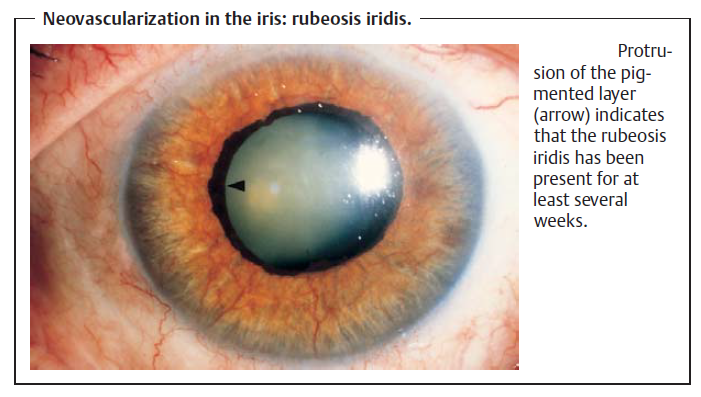
Neovascularization in the Iris (Rubeosis Iridis )
Definition: Rubeosis iridis is neovascularization in the iris that occurs in various retinal disorders.
Etiology: The most frequent causes of rubeosis iridis are proliferative diabetic retinopathy and retinal vein occlusion. Retinal periphlebitis is a less frequent cause of neovascularization in the iris.
Symptoms and diagnostic considerations: Neovascularization in the stroma of the iris is asymptomatic for the patient. Neovascularization in the angle of the anterior chamber is irreversible and produces secondary angle closure glaucoma with the typical symptoms of acute glaucoma: loss of visual acuity, intense pain, conjunctival and ciliary injection, and a “rock hard” eyeball upon palpation.
Differential diagnosis: Acute glaucoma due to other causes such as acute angle closure glaucoma should be excluded.
Treatment, prognosis, and prophylaxis: Rubeosis iridis is essentially tantamount to the loss of an eye. Usually it leads to irreversible blindness. Prompt laser treatment of retinal disorders is crucial to prevent rubeosis iridis. Secondary angle closure glaucoma is treated by transscleral freezing of the ciliary body (cyclocryotherapy) to reduce intraocular pressure. Where this fails or the eye shrinks (phthisis bulbi) and the patient experiences intense pain, enucleation of the eye is indicated.
Prompt laser treatment is important in proliferative diabetic retinopathy to prevent rubeosis iridis.
Tumors:
Malignant Tumors (Uveal Melanoma)
With an incidence of one per ten thousand, malignant uveal melanoma is the most common primary intraocular tumor. It usually occurs as a choroidal melanoma, and is almost always unilateral. Tumors in the iris are detected earlier than tumors located in the ciliary body and choroid.
- Iris melanomas: These tumors are often initially asymptomatic. However, metastatic melanoma cells in the angle of the anterior chamber can lead to secondary glaucoma. Circumscribed iris melanomas are removed by segmental
- Ciliary body melanomas: Symptoms include changes in accommodation and refraction resulting from displacement of the lens. Ciliary body melanomas are resected en bloc.
- Choroidal melanomas: These tumors become clinically symptomatic when involvement of the macula reduces visual acuity or the patient notices a shadowin his or her field of vision as a result of the tumor and the accompanying retinal detachment. The diagnosis is confirmed with the aid of transillumination, ultrasound, and fluorescein angiography. Choroidal tumors are treated with radioactive isotopes delivered by plaques of radioactive material (brachytherapy). Enucleation is indicated for tumors whose diameter exceeds 8mm and whose prominence exceeds 5mm.
- Uveal metastases most frequently develop from carcinomas of the breast or lung. They are usually flat with little pigmentation.
Benign Choroidal Tumors
Choroidal nevi occur in 11% of the population. They can lead to secondary neovascularizationwith retinal edema. In very rare cases where the macula is involved, choroidal nevi can lead to impaired vision. However, benign choroidal tumors are normally asymptomatic. iridectomy.





![[Beauty Review] The Face Shop THE THERAPY Secret-Made Anti-Aging Cream - PURPLECHIVES](https://purplechives.com/wp-content/uploads/2017/04/2017-03-30-03-52-21-1-e1491872022291-798x1024.jpg)

