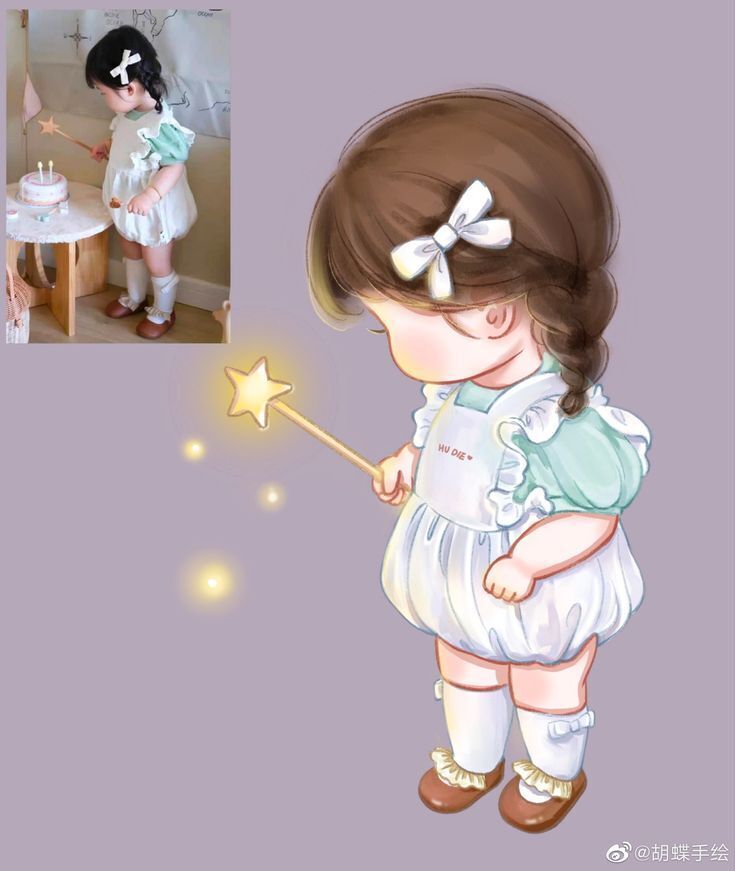
Cuộc sống công sở với những áp lực không ngừng khiến bạn cảm thấy mệt mỏi và căng thẳng? Hãy thử thư giãn với những hình vẽ cute đáng yêu mà VietnamWorks HR Insider chia sẻ dưới đây. Nó không chỉ giúp bạn giảm stress mà còn mang lại nhiều lợi ích bất ngờ cho công việc đấy!

Trong cuộc sống bận rộn của dân văn phòng, việc đối mặt với căng thẳng là điều không thể tránh khỏi. Tuy nhiên, chỉ cần một vài phút ngắm nhìn những hình vẽ cute đáng yêu có thể mang lại niềm vui bất ngờ, giảm bớt áp lực và tái tạo tinh thần. Hãy cùng VietnamWorks HR Insider khám phá cách mà hình ảnh dễ thương này trở thành “vũ khí” cải thiện hiệu suất làm việc mỗi ngày như thế nào nhé!









































































































Xem thêm:
- Những câu nói hay về cuộc sống hay nhất
- Top câu nói hay về cuộc sống vui vẻ
- Những status thả thính hài hước thú vị
- Tổng hợp các caption hài hước đăng lên bão like
- Xem thêm những câu nói hay về nhân cách sống
















Chỉ với vài phút ngắm nhìn những hình vẽ cute đáng yêu mà VietnamWorks HR Insider chia sẻ trên đây, bạn có thể “nạp” lại năng lượng tinh thần và sẵn sàng đối diện với thử thách mới. Và đừng quên tận dụng những công cụ tìm việc tại nền tảng VietnamWorks để bắt lấy những cơ hội nghề nghiệp phù hợp nhé!
>>> Xem thêm:
- Lưu ngay các mẫu hình nền điện thoại full HD 4K đẹp mắt tại đây!
- Top 100 STT hay khi đăng ảnh thú vị nhất
- Các biệt danh cho ny dễ thương
- Các hình ảnh cute anime
- Top ảnh thiên nhiên đẹp 3d
- Lưu ngay hình nền máy tính full HD
- Tìm kiếm hình xăm tay chất lừ tại đây
- Đăng ngay các ảnh đại diện Facebook ý nghĩa
— HR Insider —
VietnamWorks – Website tuyển dụng trực tuyến số 1 Việt Nam
ĐĂNG KÝ TÀI KHOẢN TÌM VIỆC
VietnamWorks là nền tảng tuyển dụng trực tuyến lớn nhất Việt Nam, với hơn 20 năm kinh nghiệm và hàng triệu ứng viên tiềm năng. VietnamWorks kết nối hiệu quả người tìm việc với các nhà tuyển dụng uy tín trên mọi lĩnh vực, giúp người tìm việc nhanh chóng tìm được công việc mơ ước. Tại VietnamWorks, người tìm việc sẽ được truy cập hàng ngàn tin tuyển dụng mới nhất, cập nhật liên tục từ các doanh nghiệp hàng đầu, tìm kiếm việc làm phù hợp với năng lực, kinh nghiệm và sở thích. Ứng tuyển dễ dàng chỉ với vài thao tác đơn giản. Đặc biệt, người tìm việc làm có thể tạo CV trực tuyến miễn phí, chuyên nghiệp và thu hút nhà tuyển dụng và nhận gợi ý việc làm phù hợp dựa trên CV và kinh nghiệm, để tìm việc nhanh chóng tại môi trường làm việc mơ ước.
Post Views: 64,447
Bài viết dành riêng cho thành viên của HR Insider.