
Tổng hợp những hình ảnh mèo đáng yêu và buồn cười nhất
Khám phá thế giới của những chú mèo với những hình ảnh độc đáo, hài hước và dễ thương nhất trong thể loại mèo buồn.
Không chỉ có những bức tranh mèo hài hước, mà còn có những tác phẩm thể hiện cảm xúc buồn. Nếu bạn đang tìm kiếm những hình ảnh mèo buồn cute và hài hước, hãy thưởng thức bộ sưu tập này.

Chia sẻ những hình ảnh mèo buồn, hài hước và dễ thương để bạn có thêm nhiều lựa chọn. Hãy xem và lưu những bức tranh mèo buồn mà bạn thích nhất!

Danh sách những bức tranh mèo buồn, hài hước và dễ thương đang chờ bạn khám phá. Hãy tận hưởng những khoảnh khắc ngộ nghĩnh với thế giới mèo.
Những bức tranh mèo buồn khiến bạn chạm vào tâm hồn

Bộ sưu tập hình ảnh mèo buồn, thấu hiểu tâm trạng

Những tác phẩm nghệ thuật mèo buồn, hài hước và dễ thương
Hình ảnh mèo buồn đáng yêu, chắc chắn làm bạn gặp nhiều cảm xúc

Bức tranh mèo buồn hài hước, chắc chắn làm bạn cười
Hình ảnh mèo thể hiện tâm trạng buồn, lạc quan
Hình chú mèo trong trạng thái buồn, nhưng vẫn rất đẹp
Bức tranh mèo buồn dễ thương, đáng yêu đến không thể cưỡng

Bức tranh mèo buồn đáng yêu xin lỗi
Hình ảnh mèo buồn cute, hài hước và dễ thương

Bức tranh mèo buồn cute, chắc chắn sẽ làm bạn cười
Hình ảnh mèo buồn dễ thương, gửi đến bạn sự ấm áp

Bức tranh mèo buồn hài hước độc đáo

Hình ảnh mèo buồn tâm trạng cảm xúc

Bức tranh đẹp về chú mèo buồn đầy nghệ thuật

Meme buồn cute, chắc chắn sẽ làm bạn cười
Meme buồn đầy chán chường

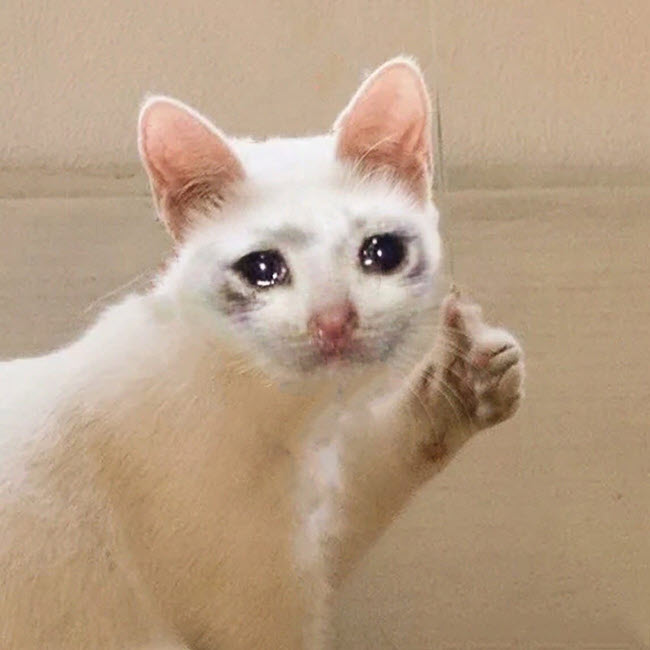
Meme buồn lạc quan

Meme con mèo buồn dễ thương
Meme chú mèo buồn hài hước

Meme hình con mèo buồn gây cười

Meme hình mèo buồn cute thú vị

Meme hình mèo buồn đẹp đến ngất ngây

Meme mặt mèo buồn hài hước cuốn hút

Meme mèo buồn thảm thiết

Meme mèo buồn cute đẹp lòng
Meme mèo buồn cute khóc xót xa

Meme mèo buồn cute, hài hước và dễ thương

Meme mèo buồn cute lạc quan

Meme mèo buồn dễ thương hết nấc

Meme mèo buồn dễ thương đến mức khó cưỡng

Meme mèo buồn đẹp ngất ngây

Meme mèo buồn hài hước nhất đời
Meme mèo buồn hài hước, dễ thương tận cùng
Meme mèo buồn hài hước đỉnh cao
Meme mèo buồn khóc cute và đáng yêu

Meme mèo buồn khóc như mưa dầm

Meme mèo buồn tỏ ra lạnh lùng
Meme mèo cảm thấy buồn dễ thương nhất

Meme mèo cute khóc đáng thương
Meme mèo dễ thương xin lỗi ngọt ngào

Meme mèo buồn đời chán chường

Meme mèo buồn nản mệt mỏi thảm thiết

Meme mèo chán đến tận cùng

Meme mèo hài hước đầy năng lượng

Meme mèo mệt mỏi đến nín thở
Meme mèo buồn cute, hài hước đáng yêu

Meme mèo buồn đầy cảm xúc

Meme mèo đáng thương tủi
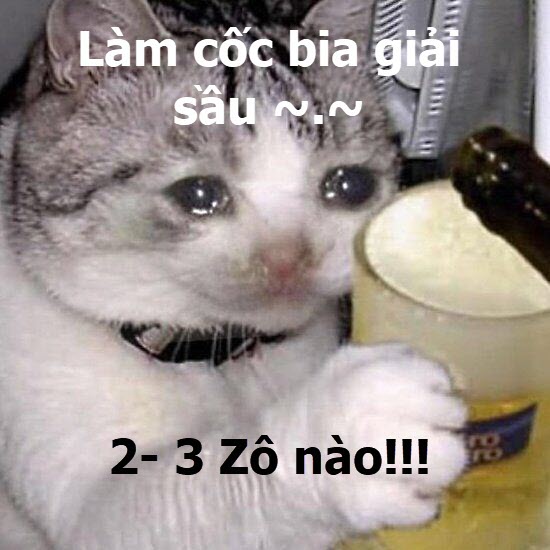
Meme mèo uống bia đầy phong cách

Mèo buồn chia sẻ cảm xúc qua meme
Như vậy, bạn vừa tham khảo nhiều meme mèo buồn cute, hài hước, dễ thương. Nếu bạn yêu thích bất kỳ meme nào, hãy lưu chúng miễn phí về máy để sử dụng khi bạn thích. Cảm ơn bạn đã quan tâm và theo dõi bài viết này.
Admin
Link nội dung: https://pi-web.eu/tong-hop-nhung-hinh-anh-meo-dang-yeu-va-buon-cuoi-nhat-1735905007-a2969.html