
Ảnh chế Meme “tấu hài” không đỡ nổi!
Sau những giờ làm việc căng thẳng thì lướt Newfeed giải trí trên Instagram, TikTok, Facebook hay 1 số trang như Haivl (giờ tạch rồi) là một hình thức được
Sau những giờ làm việc căng thẳng thì lướt Newfeed giải trí trên Instagram, TikTok, Facebook hay 1 số trang như Haivl (giờ tạch rồi) là một hình thức được nhiều người yêu thích. Không chỉ cập nhật tin tức một cách nhanh chóng, bắt trend hot mà đây còn được xem là một kho tàng giải trí khổng lồ.
Nói đến tính giải trí và hài hước, không thể không kể đến công lao to lớn của thần dân netizen. Nếu trước đây mọi người được phen thích thú với những câu nói trending thì bây giờ còn có thêm những ảnh meme nói về độ hài hước thì khỏi phải bàn.
Nghe meme có vẻ xa lạ nếu bạn không rành văn hóa internet, nhưng thật ra meme là một trào lưu chế ảnh hài hước khá quen thuộc, hãy cùng tìm hiểu về meme là gì và hình ảnh meme hot dưới đây nha!
Meme bắt nguồn từ đâu
Nói về nguồn gốc meme thật ra không bắt nguồn từ trực tuyến mà đây là thuật ngữ lần đầu tiên được sử dụng bởi tác giả Richard Dawkins trong tác phẩm The Selfish Gene vào năm 1976. Meme được sử dụng để miêu tả những ý tưởng hay các hành vi lan truyền trong khắp cộng động.
Meme là gì? Như vậy, meme là một phần của văn hoá truyền miệng, như nhắc đến câu chuyện hấp dẫn, những câu nói ví von hay trending hài hước, hay đơn giản là một câu bông đùa được mọi người thêm vào bức ảnh hợp người hợp hoàn cảnh.
Tìm hiểu về meme là gì? Những ví dụ nổi bật về meme đang hot trên internet – Nguồn ảnh: Internet
Ngày nay, meme được nhắc nhiều là meme internet, được sử dụng nhiều ở giới trẻ với nội dung hài hước, châm biếm, hay diễn tả cảm xúc có gì đó tấu hài khiến người xem không khỏi bật cười. Meme cũng có rất nhiều loại như những hình ảnh có chèn thêm chữ, hình động vui nhộn, truyện tranh, hoặc một biểu cảm “khó đỡ” của nhân vật nào đó…
Nghe thì có vẻ khó hình dung, nhưng những hình ảnh ví dụ về các meme đang hot “rần rần” dưới đây chắc hẳn không cần giải thích nhiều bạn cũng sẽ hình dung rõ hơn về trào lưu meme chưa giảm nhiệt trên mạng xã hội hiện nay.
Meme gấu trúc kinh điển
Mở đầu loạt meme hài phải kể đến meme gấu trúc được sử dụng khá phổ biến với những biểu cảm hài hước, còn được gọi là biaoqing có nguồn gốc từ Trung Quốc thường chỉnh sửa lại từ những hình ảnh của nhân vật nổi tiếng chẳng hạn như:

Bộ ảnh meme gấu trúc với vô vàn biểu cảm – Nguồn ảnh: Internet
Sau một thời gian, meme gấu trúc được cư dân mạng Việt Nam biến tấu lại với những nội dung thú vị không kém như:
“Hãy nhìn vào ánh mắt chân thành ngây thơ đáng tin này của tôi đi, tôi thật sự không lừa bạn”. Có ai nhìn xong thật sự tin gương mặt hết sức chân thành, không một chút giả dối này chưa?
“Không hề giả trân miếng nào luôn” tin tôi đi – Nguồn ành: Internet
“Sự việc không như anh nghĩ, nghe em giải thích…” Bạn có thấy câu nói này hơi quen tai không, thường có trong lời thoại của nhân vật phản diện trong phim. Nhưng bây giờ được dùng nhiều trong các comment với những tình huống đa dạng khác nhau.

Memme sự việc không như anh nghĩ… được dân mạng thường xuyên bình luận với mục đích châm biếm – Nguồn ảnh: Internet
Phòng bệnh cũng không đáng sợ và khó khăn so với việc phòng người sớm nắng chiều mưa, thay đổi nhanh như chong chóng, hay lòng người khó lường như meme này đây.
Có ai từng được bạn bè buông lời cay đắng như meme này chưa? Thật đau lòng hết sức – Nguồn ảnh: Internet
Meme một số nhân vật chẳng mấy chốc nổi tiếng bất ngờ
Meme Muhammad Akhtar Thất Vọng
Hình ảnh người đàn ông tay chống nạnh, với biểu cảm thất vọng bổng dưng được lan truyền chóng mặt vào trong thời gian gần đây với tần suất xuất hiện dày đặt trong các commnent khiến dân mạng không khỏi thích thú.

Meme Mohammad Akhtar trở thành “huyền thoại” đi đâu cũng gặp – Nguồn ảnh: Internet
Được biết, người đàn ông này có tên là Mohammad Akhtar, là người Pakistan. Đây là hình ảnh được chụp lại trong trận đấu ở bộ môn crricket, diễn ra giữa hai đội tuyển là Pakistan và Australia trong khuôn khổ giải Cricket World Cup 2019.
Ở một tình huống cầu thủ đội chủ nhà Pakistan bỏ lỡ cú bắt bóng, khiến cho chủ nhân của bức ảnh này liền tỏ thái độ thất vọng tràn trề trên khán đài. Vì vẻ mặt khiến người xem nhận xét là “tấu hài” khiến anh ta nhanh chóng nổi tiếng, chẳng những vậy còn được rất nhiều kênh thông tin phỏng vấn ghi hình.
Cho đến bây giờ, độ phủ sóng của Mohammad Akhtar qua ảnh meme cũng không phải dạng vừa đâu khi được mọi người lưu lại để dùng thanh xuân đi comment dạo bằng meme “người đàn ông thất vọng”.

Nếu bạn vô tình làm vỡ cốc mà thấy “thần thái” của mẹ bạn như thế này thì chuẩn bị tinh thần đi nhé – Nguồn ảnh: Internet
Meme bác Đa tổ trưởng
Với câu nói quen thuộc: “Tôi năm nay hơn 70 tuổi rồi mà chưa gặp một trường hợp nào nó như thế này cả…” đang là một trào lưu hot.
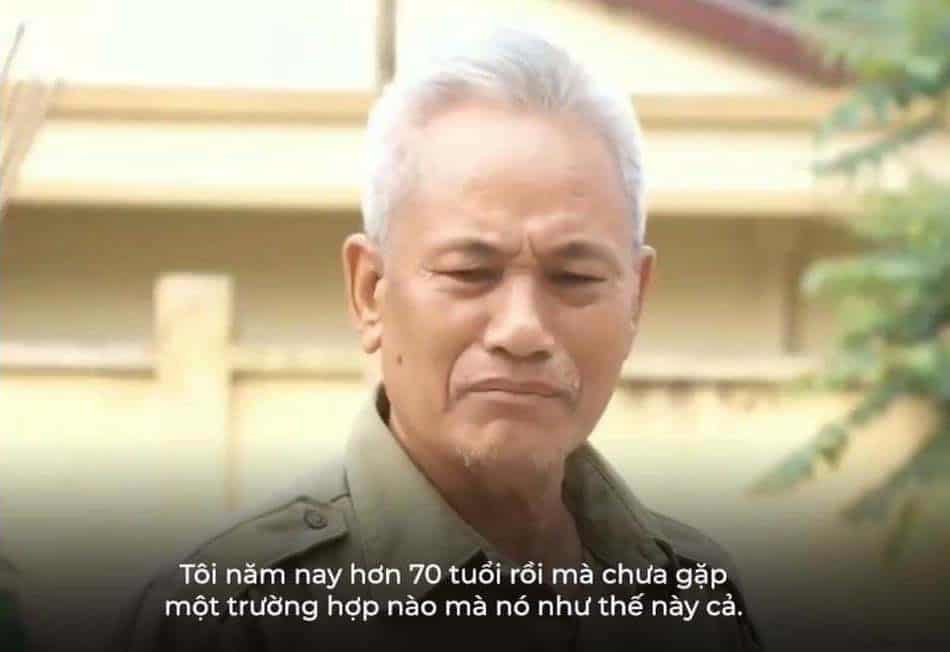
Meme bác Đa tổ trưởng được mọi người thích thú comment khá nhiều trong các bài viết – Nguồn ảnh: Internet
Về nguồn gốc meme bác Đa tổ trường bắt nguồn từ kênh youtube chính thức của truyền hình Công an Nhân dân – ANTV đã từng đăng tải một đoạn video phóng sự có tiêu đề Trần Đình Sang – kẻ ngông cuồng chống đối pháp luật là ai?
Trong đó, có đoạn phỏng vấn bác Nguyễn Hữu Đa đang là tổ trưởng bảo vệ dân phố số 5, ở phường Yên Ninh thuộc thành phố Yên Bái, bác đã phát biểu câu nói trên với những ngôn từ đời thường, bình dị nhưng tỏ rõ thái độ gay gắt của mình, vô tình tạo nên sự nổi tiếng không kịp đỡ khi lượt view tăng cao chỉ trong thời gian ngắn.
Một số meme chế lại từ hình ảnh của đoạn video trên cho thấy sự sáng tạo vô bờ bến của cư dân mạng khiến bác Đa cũng phải “cạn lời” khi nhìn thấy hình ảnh của mình.

Bác Đa sẽ có biểu cảm gì khi thấy meme này? – Nguồn ảnh: Internet
“Ủa câu này bác có nói không nhỉ?” – Nguồn ảnh: Internet
Meme bé Sa
Meme cute không thể nào không nhắc đến biểu cảm của bé Sa khi quay Vlog cùng mẹ Quỳnh. Nhờ vào hình ảnh siêu dễ thương của mình, bé Sa đã “đốn tim” không ít người.

Meme bé Sa với biểu cảm siêu cưng – Nguồn ảnh: Internet
Với kiểu đầu nấm huyền thoại, đôi mắt tròn và sáng kèm theo gương mặt vô cùng “thần thái” của mình khiến cậu bé này sở hữu không ít ảnh meme được lan truyền chóng mặt. Quan trọng nhất là cư dân mạng còn đặc biệt nhấn mạnh với caption “Sa chào cô chú đi con” là lời giới thiệu quen thuộc của Quỳnh Trần JP mẹ bé luôn nhắc nhở mỗi khi mở đầu vlog.
Một số comment hài hước của cư dân mạng về câu nói quen thuộc “Sa chào cô chú đi con”.



Một loạt biểu cảm dễ thương và caption hài hước hợp hoàn cảnh của người dùng Facebook – Nguồn ảnh: Internet
Meme tình yêu
Tất nhiên với độ thú vị cực cao của meme thì dùng meme để thả thính là một chuyện không thể nào bỏ qua. Tuy nhiên meme thả thính, hay meme tình yêu như thế nào để hợp người hợp hoàn cảnh phải dựa vào độ sáng tạo của chủ nhân meme rồi. Không để mọi người thất vọng, những meme chủ đề tình yêu phải nói là “chất phát ngất” tha hồ lưu lại để dành.
Nhắc về chủ đề tình yêu, phải kể đến hàng loạt caption thả thính siêu hài nhưng đi vào lòng người của Lân Jee chẳng hạn như:
“Lấy nét anh còn chư được, nói gì lấy em…” – Đây là một câu chuyện buồn – Nguồn ảnh: Lân Jee
Có ai “gục ngã” khi được thả thính như thế này chưa? – Nguồn ảnh: Lân Jee
“Hình như tôi chiều các em quá nên các em hư đúng không?” Đây là câu nói đang hot thời gian gần đây, hình ảnh này được rất nhiều bạn thích thú “để dành” đi “comment” dạo trên mọi mặt trận.

Meme nổi tiếng này có nguồn gốc từ tài khoản tiktok của Khoa Vương – Nguồn ảnh: Internet
Meme từ những chú mèo với những biểu cảm dễ thương cũng được rất nhiều người thích thú:
Dễ dàng tìm thấy những meme về thú cưng với caption dễ thương trên internet – Nguồn ảnh: Internet
Những meme được nhiều người thích thú về độ hài hước cao
Khi bạn xem một tin tức cực sốc nào đó và tò mò đọc những bình luận bên dưới, chắc hẳn sẽ bật cười với hình ảnh meme này vì vừa diễn tả đúng tâm trạng của mình lại vừa hài hước:
“Kính râm cũng không thể che nổi cú sốc này” – Nguồn ảnh: Internet
Khi kính râm không thể che nổi cú sốc này thì chỉ còn cách này thôi! À chỉ là vui thôi nhé, đừng làm theo.

Meme sau khi nhìn post của bạn, đôi mắt tinh anh này không còn thiết tha nhìn cái gì nữa – Nguồn ảnh: Internet
Khi bạn muốn tìm một meme thể hiện sự kinh ngạc thì meme với tiêu đề “Gì ghê vậy” ảnh Tiểu Long Nữ Lưu Diệc Phi mặt Lương Bổng Người Phán Xử này được chế lại cũng rất hợp hoàn cảnh:
Nhìn meme này muốn “xỉu up xỉu down” – Nguồn ảnh: Internet
Ngày nay, không chỉ mua hàng mới cần chốt đơn mà còn có nhiều tình huống khiến mọi người tranh nhau chốt đơn với meme hình ảnh cô bé Hyeri trong “gia đình là số một” với biểu cảm “đanh đá” và câu nói quen thuộc: “Tất cả là của tao”.

Ai có ba bích, ai có sổ hộ nghèo được quyền ưu tiên “chốt đơn” trước là ý nghĩa của meme này – Nguồn ảnh: Internet
Nếu ngày trước nhiều người có thói quen comment để lại “.” để khỏi trôi bài thì bây giờ không ít người lại thay thế bằng cách để lại meme này khi nào rảnh lại vào hóng hớt tin hot.

Không khỏi bật cười vì tính độ hài hước của comment này – Nguồn ảnh: Internet
“Đâu, ai biết gì đâu” Nghe có vẻ ngây thơ nhưng được dùng nhiều trong các comment với biểu cảm “Ngây thơ vô số tội”. Nhưng không thể phủ nhận đây là meme dễ thương hết sức.
Gương mặt ngây thơ vô số tội – Nguồn ảnh: Internet
Cứ đến hẹn lại lên, mỗi năm sau kỳ thi THPT Quốc Gia hay công bố điểm thi thì meme “thi cử” lại nổi lên như cồn. Nhưng thí sinh xem vui thôi đừng, đừng tụt mood nhé!
Tranh thủ tuyển dụng thì thời cơ tới, meme có nguồn gốc từ Lộc Fuho – Nguồn ảnh: Internet
Câu chuyện mỗi sáng thức giấc để bắt đầu ngày mới, chuẩn bị đi học, đi làm luôn cần một ý chí “phi thường”, đối với meme anime này quả thật nói lên nổi lòng của không ít người.
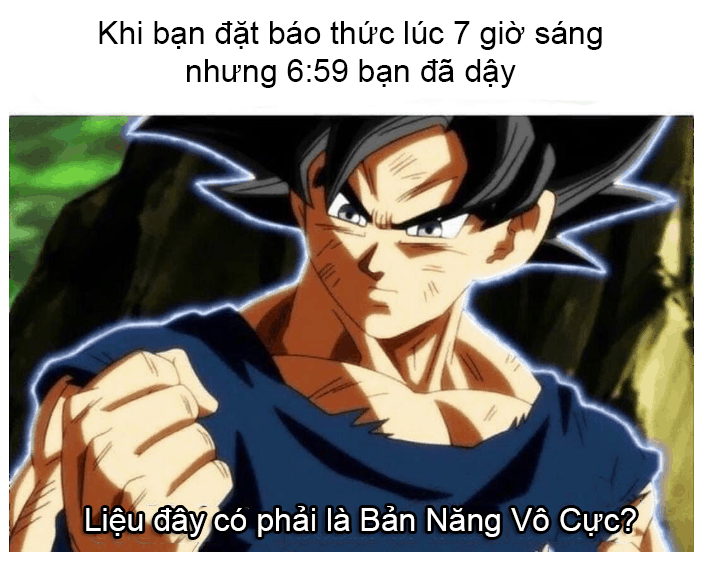
Có ai cảm thấy mình thật phi thường không? – Nguồn ảnh: Internet
Meme với hình ảnh mang đậm chất “Made in Việt Nam” được biến tấu lại với phong cách tương tự Biaoqing, nhưng lại thay thế bằng những hình ảnh đặc trưng Việt Nam như chiếc nón lá, dép tổ ong đang khá đông netizen Việt đón nhận vì độ hài hước. Mặc dù cũng có một số nhận xét về câu từ vẫn chưa mượt lắm nhưng vẫn không phủ nhận tinh thần sáng tạo của tác giả bộ ảnh này.

“Lông ngỗng rải đầy đất” có khiến bạn liên tưởng đến câu chuyện nào không – Nguồn ảnh: Internet

Khi bạn muốn kết thúc câu chuyện tại đây và rồi cách giải quyết là nhấn nút “send” meme này – Nguồn ảnh: Internet
Trong một cuộc trò chuyện đôi khi có chút nhàm chán, hay khi bạn muốn giải toả căng thẳng thì meme quả thực là “một chất xúc tác” gây tiếng cười cực thoải mái. Đôi khi, trong những comment, không thể phủ nhận xem được những meme hài hước khiến không ít người cảm thấy cực kỳ thư giãn. Vậy bạn đã bao giờ dùng meme để comment hay inbox chưa, những meme yêu thích của bạn là gì? Hãy chia sẻ cho mọi người cùng vui nha!
Admin
Link nội dung: https://pi-web.eu/anh-che-meme-tau-hai-khong-do-noi-1735897216-a2943.html