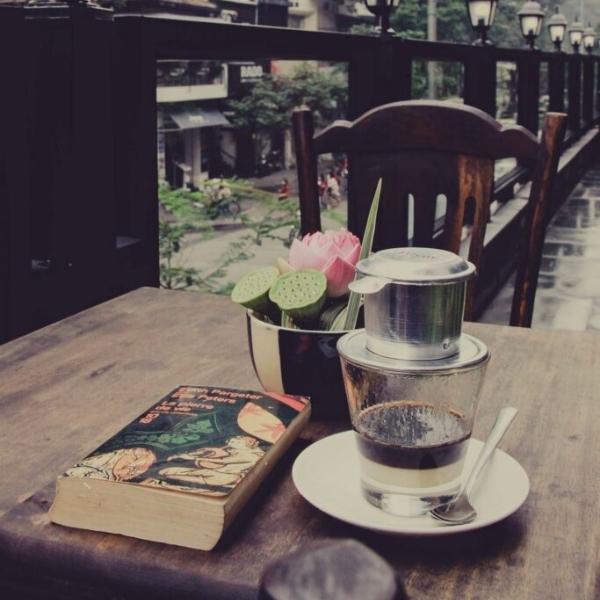
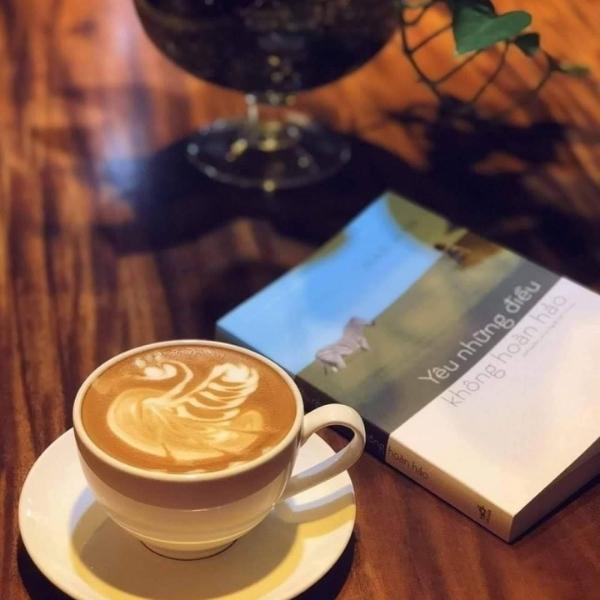
Hình ảnh cà phê một mình kèm chiếc caption để đăng mạng xã hội. Đây là một cách giải tỏa tâm trạng hiệu quả. Khi sử dụng hình ảnh này họ chỉ tồn tại một mong muốn sẽ có ai đó tới để họ không còn thấy cô đơn. Nhưng không bắt buộc ai cũng mang thể uống được cà phê và cũng không bắt buộc ai cũng có thể chụp được 1 tấm hình đẹp.






Xem thêm: 60+ Hình ảnh ly cà phê đẹp
























Xem thêm: 90+ Hình ảnh ly trà sữa đẹp





















Xem thêm: 50+ Hình ảnh ly bia buồn



















Xem thêm : 90+ Hình ảnh ly rượu buồn
Cửa hàng thủy tinh Luminarc chuyên cung cấp các mặt hàng sản phẩm ly thủy tinh chất lượng. Với tiêu chí đặt uy tín lên hàng đầu, chúng tôi cam kết mang đến cho các khách hàng những sản phẩm chân thật, mẫu mã đa dạng, giá cả cạnh tranh. Quý khách có thể đến xem hàng trực tiếp tại showroom của chúng tôi tại địa chỉ dưới đây:
Website: https://thuytinhocean.net/
Địa Chỉ: 439 Đ. Cách Mạng Tháng 8, Phường 13, Quận 10, Thành phố Hồ Chí Minh
Mail: [email protected]
Phone: 094 7836 567



![[Tổng hợp] 496+ Ảnh Yuno Gasai anime, sexy mới nhất hiện nay](https://hutbephottanphat.vn/wp-content/uploads/2024/12/anh-yuno-gasai-sexy-24.jpg)







