
In this article, we will address thrombosis in peripherally inserted central catheters (PICCs) based on the following aspects: incidence, causes, physiology, symptomatology, and prevention.
What is thrombosis?
Thrombosis is the formation of a clot in a vessel. It can be particularly serious when the thrombus migrates, which can lead to pulmonary embolism.
GAVeCeLT provides the following definition for catheterization-related thrombosis:
“Catheterization-related thrombosis means that the tract in which the catheter is inserted has venous thrombosis due to endothelial injury caused by penetration of the catheter into the vein or by mechanical and/or chemical trauma caused by the catheter tip on the endothelium.”
GAVeCeLT also adds that it is important to differentiate thrombosis from catheter obstruction. In fact, the latter is caused by clots or by the misnamed fibrin cuff, which is actually fibroblasts that respond to the presence of a foreign body (the catheter).
There are two types of catheterization-related thrombosis:
– Superficial venous thrombosis, when the affected vessels are shallow, such as those in the upper and lower limbs.
– Deep venous thrombosis, when the affected vessels are deep, such as the subclavian, brachiocephalic trunk, and superior vena cava, for example.
An important fact to remember is that an occluded catheter does not imply that there is a thrombosis. In fact, a thrombus is the formation of a clot in the vein. However, a clot may form in a catheter without it being a thrombosis.
The incidence of thrombosis in PICCs
The widespread use of PICCs has led to their increasingly poor reputation as a thrombosis generator. Indeed, several studies have shown that PICCs have a higher rate of thrombosis than central catheters in general.
According to the Spanish Society for Medical Oncology (SEOM) document “Prophylaxis and treatment of central venous catheter-associated thrombosis”:
The incidence of venous thromboembolic disease (VTD) in the oncology patient varies between 0.8 and 30%, depending on the series, and depends on various factors related to the patient, the tumour, and the type of treatment. Cancer patients have a higher risk of suffering a thrombotic event than the general population […].
In his article on PICC-related thrombosis, Chopra notes that the incidence of deep vein thrombosis (DVT) for PICCs is between 5% and 15% for inpatients and between 2% and 5% for outpatients.
Studies examining PICC-related deep vein thrombosis while maintaining weekly follow-up, irrespective of the presence of symptoms, report deep vein thrombosis rates of up to 33%.
However, Dr. Mauro Pittiruti has emphasized on several occasions (congresses, interviews), that certain important studies in this regard were biased and that, in fact, this incidence is linked to the insertion technique in almost all cases.
We can therefore deduce that, if the procedure is performed as carefully as possible and if we take into account the several factors that we will discuss below, the incidence of thrombosis in PICC lines can be greatly reduced, as already been demonstrated by the Vassorano publication from the GAVeCeLT group.
Causes of catheter-related thrombosis (CRT)
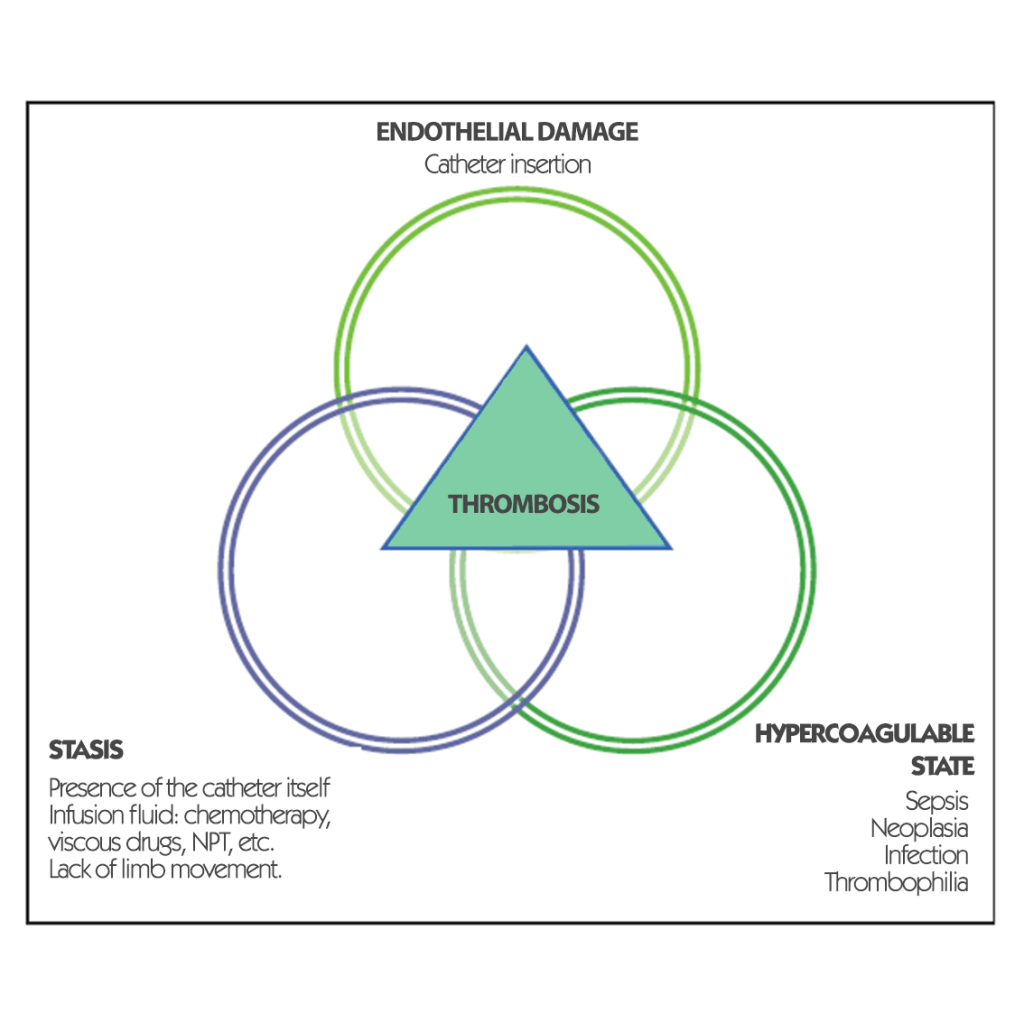
In the article “Catheter-related thrombosis: A practical approach” that looks at ICU patients and discusses central catheters and PICCs used in this setting, the mechanisms leading to CRT are classified according to three categories:
During the 2019 SEINAV congress, Nancy Moureau explained the causes of deep vein thrombosis as follows:

In the study “Incidence and risk factors of superficial and deep thrombosis in paediatric PICCs” (Menéndez et.al), two interesting data appear:
– According to Poiseuille’s law, the higher the catheter/vein ratio, the higher the risk of blood stasis. And consequently, according to Virchow’s triad, the greater the risk of thrombosis.
– Deep vein thrombosis is less frequent in children and arises due to expansion of the DVT thrombus.
Pathophysiology
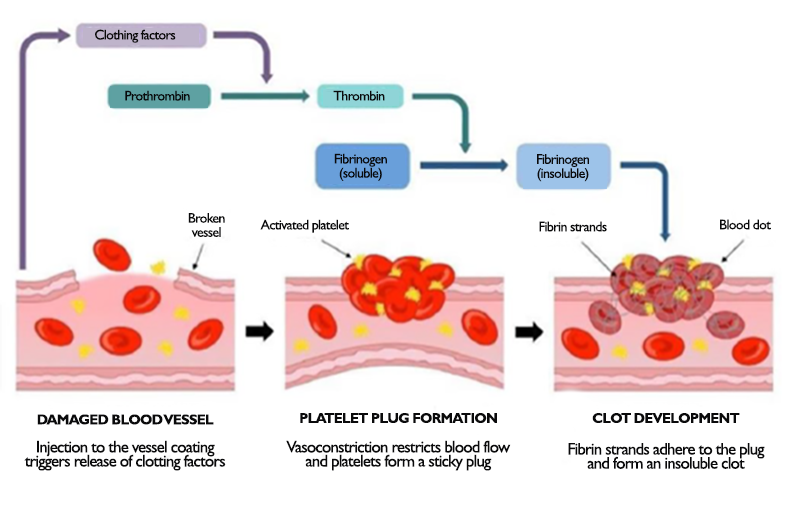
As we have seen above, a key factor in the incidence of thrombosis is the endothelial trauma that occurs at the time of insertion.
In fact, thrombus formation always corresponds to a response of the body to an aggression:
Several representative symptoms indicate the presence of thrombosis:
– Oedema of the arm (or shoulder)
– Erythema
– Ipsilateral pain (arm, shoulder, neck, face corresponding to the side of the catheter).
– Symptoms of SVC obstruction
– Difficulty drawing blood from the catheter
The number of asymptomatic patients can be significant, and in such cases, thrombosis is only detected by chance during another examination.
How to prevent thrombosis in patients with PICC lines
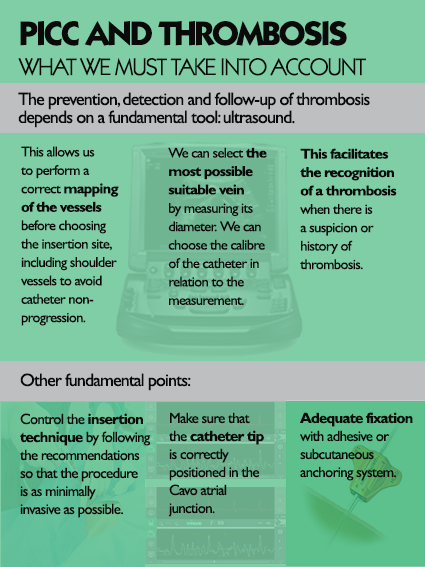
In its manual on PICC and Midline, GAVeCeLT indicates that it is possible to prevent thrombosis as follows:
– Use silicone or PUR catheters.
– Do not place a PICC near or on the same side as a recent thrombosis.
– Choose a vein at least three-times the diameter of the catheter, a factor that is especially important in children (Menéndez et.al).
– Always use ultrasound to minimize the invasiveness of the insertion as much as possible.
– Ensure that the tip is at the level of the cavoatrial junction and positioned downwards.
– Use systems that allow adequate fixation of the catheter: sutureless device + transparent dressing.
GAVeCeLT also points out that, obviously, coagulation disorders (congenital or acquired) are an independent factor directly influencing thrombosis and cannot always. be prevented. Therefore, prophylaxis with low molecular weight heparin is possible only in selected patients: history of catheterization-related thrombosis, congenital thrombophilia, history of thrombosis of various types due to pathologies with associated thrombotic risk, etc….
On the other hand, the Michigan Risk Score to Predict Peripherally Inserted Central Catheter-Associated Thrombosis study has allowed the development of a scale to establish a patient’s risk of developing thrombosis. The risk is calculated using the following variables:
– Presence of another central catheter when the PICC line is placed – 1 point.
– Leukocytes < 12,000 at the time of insertion – 1 point
– Active cancer – 2 points
– Number of PICC lines: 1 and 2 lines – 2 points; 3 and 4 lines – 3 points
– History of thrombosis – 2 points and if within the previous 30 days – 3 points.
Based on data analysed as part of a multicentre observational study involving more than 23,000 patients (in 51 hospitals), four groups have been created according to risk level:
– Class I patients: 0 points = 0.9% risk.
– Class II patients: 1-2 points = 1.5% risk
– Class III patients: 3-4 points = 2.6% risk
– Class IV patients: >4 points = 4.5% risk
Bibliography
- The risk of venous thromboembolism associated with peripherally inserted central catheters in ambulant cancer patients Jones et al. Thrombosis Journal 2017
- Peripherally inserted central catheter (PICC)-related thrombosis in critically ill patients Zochios et al J Vasc Access 2014;
- The Michigan Risk Score to Predict Peripherally Inserted Central Catheter-Associated Thrombosis Chopra, J Thromb Haemost. 2017
- The GAVeCeLT Manual of PICC and Midline Pittiruti y Scoppettuolo 2017
- Ponencia Deep Vein Thrombosis and Vascular Access, a difficult coexistence Nancy Moureau – Congreso SEINAV 2019
- Peripherally inserted central catheter (PICC)-related venous thrombosis Chopra 2020
https://www.uptodate.com/contents/peripherally-inserted-central-catheter-picc-related-venous-thrombosis - Entrevista a Mauro Pittiruti 2019
https://www.youtube.com/watch?v=10m2TdbLru0 - Ponencia The GAVeCeLT bundle for prevention of catheter-related upper extremities and central venous thrombosis Mauro Pittiruti
https://www.improvepicc.com/uploads/5/6/5/0/56503399/gavecelt_bundle_for_prevention_of_thrombosis.pdf
Articles written by the VascuFirst team







